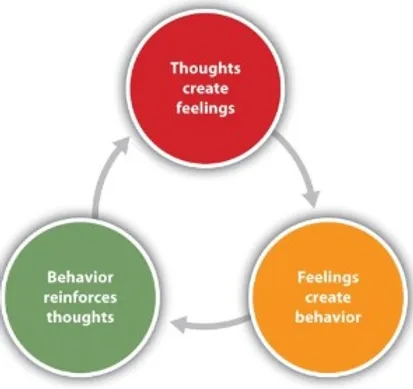
Cognitive Behavioral Therapy (or, CBT) is one of the most successful ways to treat depression outside of medication. I have experienced a lot of it through individual therapists, residential treatment, partial hospitalization (PHP), and intensive outpatient therapy (IOP).CBT is the premise that our thoughts cause our feelings which then cause our behavior. Our behavior causes more thoughts which cause more feelings and so on. Presumably, if we can change our thoughts, we will change our feelings and behavior. We may not be able to control the situations that pop up in our lives that cause the thoughts to begin with. But CBT empowers us to take control over our mind and actions. Or, as Anna Napowan said, “In a nutshell, the CBT approach works by identifying, evaluating, and finding new ways to respond to automatic thought patterns.”
CBT occurs as talk therapy one-on-one with a therapist, in a group setting, online, or through self-help books and podcasts. According to NHS, CBT can help with a whole host of other things besides for depression. CBT is applicable to those who suffer from schizophrenia, bipolar disorder, anxiety and panic disorders, obsessive compulsive disorder, borderline personality disorder, and/or phobias. CBT may not be as suitable for people who experience chronic pain and illness or who have underlying complex trauma that they have not processed through. CBT teaches strategies that focus on the capacity someone has to change themselves. You are responsible for yourself.
CBT is not easy. It takes education and lots of practice. But it is effective. I’ll show you some tools and strategies that you can use later on. Don’t forget to also check out the mental health resources page where you can find these as well.